For rehab clinicians, the relevance of postural control is significant, particularly during infant and toddler development.
Postural control:
- Develops to sustain life and to optimize attention and to support learning and function.
- Provides the stability needed to liberate the limbs and head to explore and move.
- Acquisition begins at the head and neck and progresses to the toes.
- Acquisition begins with extension of the neck and trunk muscles against gravity, soon balanced by neck and trunk flexion.
- Deficits have been identified as a significant concern in children with cerebral palsy.
- The reliance on the tonic recruitment of limb muscles to compensate for a core stability deficit has not yet been investigated.
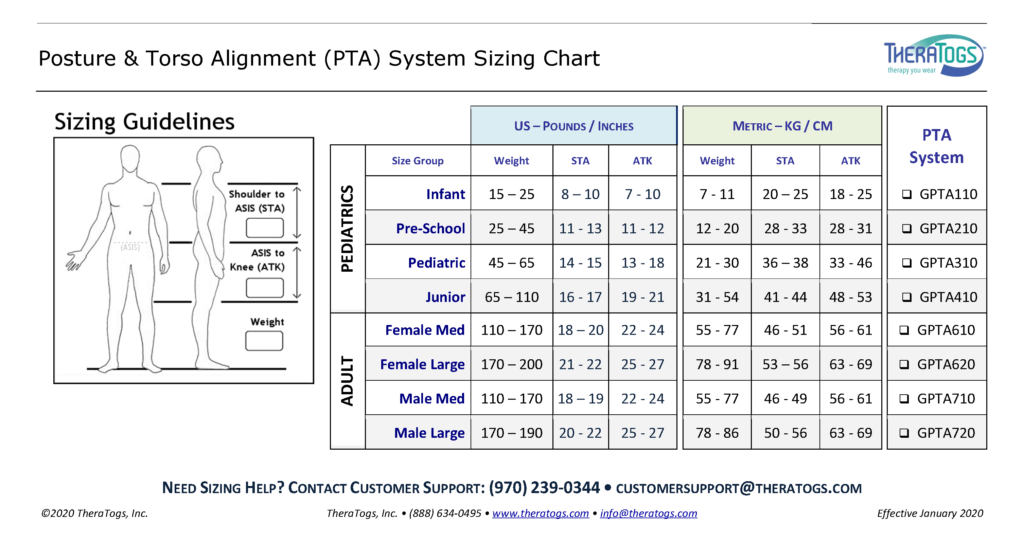
These references all speak to the importance of proper trunk alignment – the explicit purpose of the TheraTogs PTA System:
Babik I, Galloway JC, Lobo MA. 2017. Infants born preterm demonstrate impaired exploration of their bodies and surfaces throughout the first 2 years of life. Phys Ther. 97(9):915-925.
Bly L. 2011. Components of Typical and Atypical Motor Development. Neurodevelopmental Treatment Association; www.ndta.org
Boxum AG, van Balen LC, Dijkstra LJ, et al. 2014. Postural adjustments in infants at very high risk for cerebral palsy before and after developing the ability to sit independently. Early Hum Dev. 90(9):435-41.
Brogren E, Hadders-Algra M, Forssberg H. 1998. Postural control in sitting children with cerebral palsy. Neurosci Biobehav Rev. 22(4):591-6. Review.
de Graaf-Peters VB, Blauw-Hospers CH, Dirks T, et al. 2007. Development of postural control in typically developing children and children with cerebral palsy: possibilities for intervention? Neurosci Biobehav Rev. 31(8):1191-2000. Review.
Dudek-Shriber L, Zelazny S. 2007. The effects of prone positioning on the quality and acquisition of developmental milestones in four-month-old infants. Pediatr Phys Ther. 19(1):48-55.
Dusing SC, Harbourne RT, Lobo MA, et al. 2019. a physical therapy intervention to advance cognitive and motor skills: a single subject study of a young child with cerebral palsy. Pediatr Phys Ther. 31(4):347-352.
Dusing SC, Izzo TA, Thacker LR, Galloway JC. 2014. Postural complexity differs between infant born full term and preterm during the development of early behaviors. Early Hum Dev. 90(3):149-56. Free PMC article.
Dusing SC, Thacker LR, Galloway JC. 2016. Infant born preterm have delayed development of adaptive postural control in the first 5 months of life. Infant Behav Dev. 44:49-58.
Feldman AG. 2016. The Relationship Between Postural and Movement Stability. Adv Exp Med Biol. 957:105-120. Review.
Gramsbergen A, Hadders-Algra M. 2005. Posture in the picture: on the relevance of postural control in children with developmental motor disorders. Summer, 2004. Groningen, The Netherlands. Neural Plast. 12(2-3):73-75. Free PMC article.
Green EM, Mulcahy CM, Pountney TE. 1995. An investigation into the development of early postural control. Dev Med Child Neurol. 37(5):437-48.
Hadders-Algra M, Brogren E, Forssberg H. 1998. Development of postural control–differences between ventral and dorsal muscles? Neurosci Biobehav Rev. 22(4):501-6. Review.
Hadders-Algra M, Carlberg EB. 2008. Postural Control: A Key Issue in Developmental Disorders (Clinics in Developmental Medicine), MacKieth Press (Wiley).
Hadders-Algra M. Neurosci Biobehav Rev. 2018. Early human motor development: From variation to the ability to vary and adapt. 90:411-427. Free article. Review.
Heathcock JC, Galloway JC. 2009. Exploring objects with feet advances movement in infants born preterm: a randomized controlled trial. Phys Ther. 89(10):1027-38. Free PMC article. Clinical Trial.
Hirabayashi S, Iwasaki Y. 1995. Developmental perspective of sensory organization on postural control. Brain Dev. 17(2):111-3.
Johnston MV. 2009. Plasticity in the developing brain: implications for rehabilitation. Dev Disabil Res Rev. 15(2):94-101.
Konishi Y, Takaya R, Kimura K, et al. 1994. Development of posture in prone and supine positions during the prenatal period in low risk preterm infants. Arch Dis Child Fetal Neonatal Ed. 70(3):F188-91. Free PMC article.
Lee HM, Galloway JC. 2012. Early intensive postural and movement training advances head control in very young infants. Phys Ther. 92(7):935-47. Clinical Trial.
Lobo MA, Kokkoni E, Cunha AB, Galloway JC. Infants born preterm demonstrate impaired object exploration behaviors throughout infancy and toddlerhood. Phys Ther. 2015;95(1):51-64.
Monterosso L, Kristjanson L, Cole J. 2002. Neuromotor development and the physiologic effects of positioning in very low birth weight infants. J Obstet Gynecol Neonatal Nurs. 31(2):138-46. Review.
Rocha NA, dos Santos Silva FP, de Toledo AM, Tudella E. 2009. Variability in the levels of postural control in 0-4-month-old infants. Infant Behav Dev. 32(4):376-80.
Rocha NA, Tudella E. 2008. The influence of lying positions and postural control on hand-mouth and hand-hand behaviors in 0-4-month-old infants. Infant Behav Dev. 31(1):107-14.
Steindl R, Kunz K, Schrott-Fischer A, Scholtz AW. 2006. Effect of age and sex on maturation of sensory systems and balance control. Dev Med Child Neurol. 48(6):477-82.
Sweeney JK, Gutierrez T. 2002. Musculoskeletal implications of preterm infant positioning in the NICU. J Perinat Neonatal Nurs. 16(1):58-70.Review.
Vaivre-Douret L, Ennouri K, Jrad I, Garrec C, Papiernik E. 2004. Effect of positioning on the incidence of abnormalities of muscle tone in low-risk, preterm infants. Eur J Paediatr Neurol. 8(1):21-34. Clinical Trial.
van Balen LC, Dijkstra LJ, Dirks T, Bos AF, Hadders-Algra M. 2019. Early Intervention and Postural Adjustments During Reaching in Infants at Risk of Cerebral Palsy. Pediatr Phys Ther. 31(2):175-183.
van Balen LC, Boxum AG, Dijkstra LJ, et al. 2018. Are postural adjustments during reaching related to walking development in typically developing infants and infants at risk of cerebral palsy? Infant Behav Dev. 50:107-115.